Year by year, resistance to extending Medicaid to more low-income Americans in conservative states has given way. That trend seems likely to continue into 2020.
In some states, Democratic governors who favor expansion have replaced Republicans who were stalwart opponents. GOP critics have had a change of heart in some holdout states. And in several Republican-led states, citizen ballot initiatives are driving expansion.
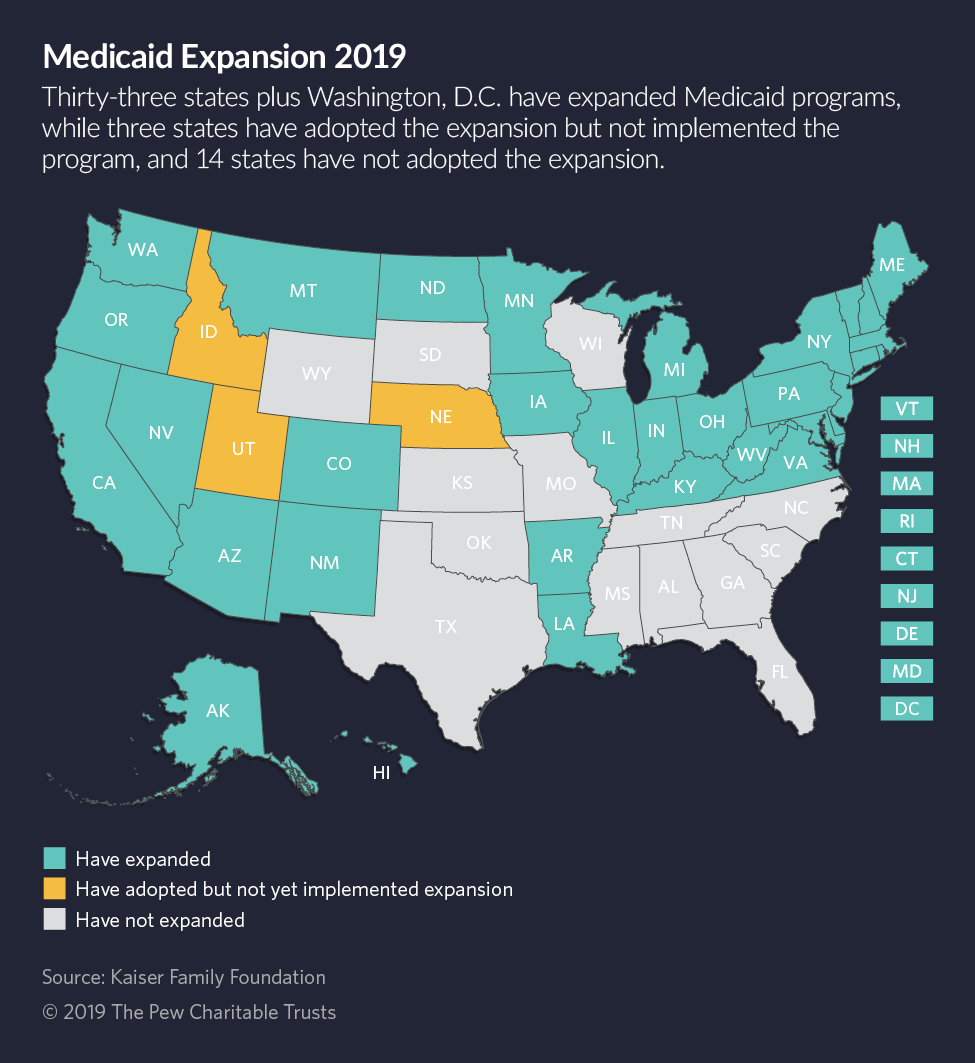
Serious efforts are underway in Kansas, Missouri, North Carolina and Oklahoma that could add them to the 36 states, plus Washington, D.C., that have opted to expand Medicaid under the Affordable Care Act (ACA), also known as Obamacare. Three of those states adopted the expansion but have yet to implement the program.
Organizers in Missouri say they have collected a quarter of the 172,000 signatures they need to get a measure on the ballot next year. In Oklahoma, organizers say they have turned in 135,000 more signatures than required.
Proponents also are optimistic about a legislative breakthrough in Kansas, where Democratic Gov. Laura Kelly is finishing up her first year in office and expansion missed by a single vote this year in a Senate committee. And in North Carolina, a new Democratic governor and a Republican-led legislative effort give expansion the best chance it’s had in that state.
In Maine, Democratic Gov. Janet Mills in January signed an executive order implementing Medicaid expansion, which had been approved by voters in 2017 but blocked by her Republican predecessor. And in Montana, Democratic Gov. Steve Bullock in May signed a law extending Medicaid expansion for another six years.
Meanwhile, Idaho, Nebraska and Utah have submitted applications to the federal government to expand Medicaid after voters approved ballot initiatives last year.
History may be repeating itself. Although Congress created Medicaid in 1966, it was another 16 years before every state agreed to participate in the government health plan for lower-income Americans. In 1982, Arizona became the last state to sign up.
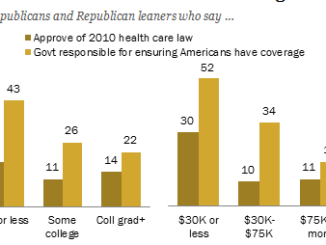
The politics surrounding the issue have changed dramatically in the past five years. Republican officeholders have shown an increasing willingness to break with party orthodoxy to support expansion. And the benefits of expansion have been thoroughly researched and publicized: Millions of Americans have gained coverage in expansion states, while rural and safety net hospitals have benefited from the additional federal resources.
Republican officeholders also have seen voters in red states signal their support for expansion at the ballot box.
In Mississippi, Democratic gubernatorial candidate Jim Hood championed expansion during his campaign. He eventually lost, but observers believe the issue helped him run a surprisingly close race against Republican Tate Reeves.
Although Kentucky has already expanded Medicaid, the winning Democratic gubernatorial challenger, Andy Beshear, made protection of the ACA a central feature of his campaign. His Republican opponent, incumbent Gov. Matt Bevin, is an outspoken opponent of the ACA. Beshear’s victory also is likely to mean that the state will stop trying to impose work requirements on Medicaid beneficiaries, a Bevin initiative.
Even Georgia’s conservative governor, Republican Brian Kemp, who highlighted his opposition to expansion in his 2018 campaign against Stacey Abrams, has softened. Earlier this week, he unveiled his own modified Medicaid expansion plan.
If not quite a conservative bandwagon, momentum is certainly moving in one direction, and policymakers in non-expansion states are taking note.
“People in Missouri know that other states right next door have passed it,” said Connie Farrow, spokeswoman for Healthcare for Missouri, the group leading the signature-gathering for that state’s ballot initiative. “Nebraska is a conservative state, and they passed it. Arkansas is a conservative state, and they passed it. Conservative states like Idaho and Utah, they’ve passed it.”
The experience states have had with expansion has made it harder to continue to stand against it, said Jesse Cross-Call, a senior health policy analyst with the Center on Budget Policy and Priorities, a liberal-leaning research and policy institute in Washington.
“There’s been a ton of evidence showing large gains in health care coverage, while helping states economically and keeping rural hospitals open,” Cross-Call said. “And it hasn’t hurt state budgets. It remains a really good deal for states to cover hundreds of thousands of people.”
New research this summer also makes the case that Medicaid expansion is literally a life-or-death decision for states. A study by the National Bureau of Economic Research found that at least 19,200 lives of adults aged 55 to 64 had been saved in states that had expanded Medicaid between 2014 and 2017.
At the same time, 15,600 people in that demographic died because their states hadn’t expanded. The deaths and non-deaths related to whether people with treatable chronic conditions, such as diabetes, heart disease and cancer, had access to health care.
It’s not just research that has made Medicaid expansion more palatable for Republican lawmakers, said Chris Pope, a health policy analyst with the Manhattan Institute, a free market policy center.
“As time goes by, the extent to which [Medicaid expansion] is associated with the Obama administration is weakening,” he said. “That makes it easier for Republicans in red states to move closer to expansion without being seen as complicit with Obamacare.”
“Plus,” Pope added, “the money is so attractive.”
Nevertheless, some Republicans are holding fast against expansion, warning that it is a financial risk their states can’t afford to take.
Missouri state Rep. Cody Smith, the Republican chairman of the House Budget Committee, told The Joplin Globe in August that he was “gravely concerned” about the Medicaid expansion initiative in his state. Missouri already spends a third of its budget on Medicaid, he pointed out. Smith did not respond to a message seeking comment.
“If we obligate ourselves to spend more money on Medicaid, those dollars have to come from other programs,” including education, Smith told the paper.
Red States Trickle In
Medicaid expansion was supposed to be a settled political issue after the Affordable Care Act passed in 2010. That’s because the law called for all states to expand Medicaid, offering eligibility to any adult earning up to 138% of the federal poverty line ($17,236 annual income for an individual), even those without children or a disability.
Federal and state governments share the financial burden of Medicaid, but Washington, D.C.’s share for the expansion population is higher than what it provides for the non-expansion Medicaid population. In the first years, the federal government paid 100% of the costs of the Medicaid expansion population. Starting next year, the federal match will be 90%.
The U.S. Supreme Court upended the original plan regarding expansion. In a 2012 ruling that otherwise upheld the ACA, the court made Medicaid expansion optional for states.
States with Democratic governors and legislatures signed up for the expansion for the start of its implementation in January 2014. A few Republican-led states, including Arizona, Michigan and Ohio, also joined immediately. Since then, red states have trickled into the expansion fold — including the three states that held initiatives last year and Montana. All are awaiting final federal approval.
And, if expansion proponents have their way, that trend will continue next year.
Donny Lambeth, a state representative in North Carolina, is among those Republican officeholders who have had a change of heart regarding expansion. He introduced a measure in the North Carolina House that would expand Medicaid, though with several wrinkles that depart from the plan by Democratic Gov. Roy Cooper.
Chief among those differences is a requirement that enrollees either work or enroll in a school or job training program. Lambeth also would raise taxes on hospitals to pay for the state’s increased Medicaid expenses.
“These are proud people who are working and want to take care of their families, but they can’t afford private insurance,” Lambeth said. He added that the trend of rural hospitals closing will continue unless expansion passes.
Eleven rural hospitals have closed in North Carolina since 2007, according to the North Carolina Rural Health Research Program at the University of North Carolina. Across the country, the program says 161 rural hospitals have shut their doors since 2005.
Support for expansion in North Carolina has come at the local level as well. The county commission in rural Graham County, by the Tennessee border, voted in September to urge the legislature to pass expansion.
“Republican leadership in the state just took the national Republican stance on it and opposed it just because it was something the Democrats had pushed,” said Dale Wiggins, the Republican chairman of the GOP-majority commission. “People doing what their political party wants rather than what the people of this country needs — that’s wrong.”
In Oklahoma, Republican lawmakers haven’t budged noticeably on expansion, but proponents got a boost in September when the former speaker of the House, Kris Steele, a Republican who had been wary of the ACA while in office, came out in favor of expansion at a town hall meeting.
“I believe [expansion] improves lives of working individuals and gives them an opportunity to be healthy and ultimately flourish in society,” Steele said in an interview. “From a conservative aspect of it, I think it makes sense for Oklahoma to have our own tax dollars to come back to our state to help out citizens.”
Strongest Prospects in Kansas
Prospects for expansion are likely strongest in Kansas. The legislature passed expansion in 2017, only to have the bill vetoed by then-Gov. Sam Brownback, a Republican. This year, the House passed an expansion bill in its legislative session but a Senate committee came up one vote shy of moving the measure to the floor.
Democratic Gov. Laura Kelly has redoubled efforts for passage next year. At the same time, Republican Senate Majority Leader Jim Denning has promised to put out his own expansion bill and has asked a special Senate committee to explore the issue.
In an interview with Stateline, Kelly said she is confident expansion will pass next year. “This is a huge issue in Kansas,” she said. “Everybody is up for re-election in 2020, and I think it is essential that this gets passed if they stand any chance of getting re-elected.”
Although the Trump administration has reviled both the ACA and Medicaid expansion, the Manhattan Institute’s Pope says that the administration’s actions may have pushed Republicans to seek expansion. From the beginning, the administration has encouraged states to customize their Medicaid programs, for example by requiring beneficiaries to work.
Conservative states such as Arkansas and Kentucky fashioned their expansion applications to the federal government around such proposals.
“The Trump administration by expanding options has made it more attractive to states,” Pope said.
A federal judge earlier this year threw out work requirements in Arkansas, Kentucky and New Hampshire. Those cases have been appealed. Arizona and Maine have both suspended plans to implement work requirements, and Democratic governors in Michigan and Virginia have raised alarms about carrying them out in their states.
The administration may want to give states flexibility in running their Medicaid programs, but it has also made clear it has no interest in encouraging expansion.
When Utah’s Republican governor and lawmakers this year tried to do a limited expansion that would have extended Medicaid eligibility only to residents with incomes below the poverty line, the Trump administration said it would not pay the higher federal match for a partial expansion. It said it didn’t want to encourage more states to expand Medicaid, even partially.
Michael Ollove covers health care for Pew Trust’s Stateline.